Conquer Your Chronic Pain Video
May 10, 2016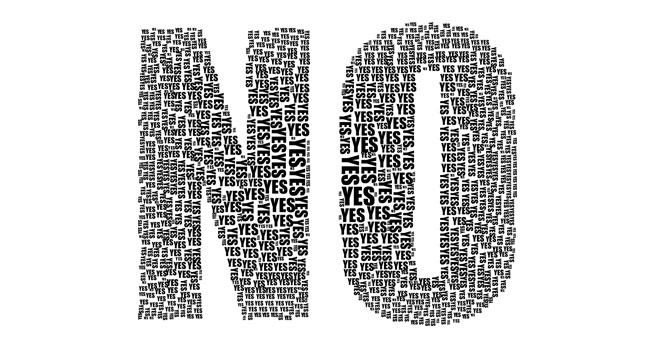
When Your Doctor Says No: Tips For Surviving The Opioid Crackdown
September 19, 2016“You never really understand a person until you consider things from his point of view…until you climb in his skin and walk in it.” That was the immortal advice given by Atticus Finch to Scout in the classic American novel “To Kill a Mockingbird” by the late Harper Lee. Scout’s journey would eventually become impactful, leading her to break down many stereotypes and preconceptions along the way, but only after she learned to see things from the perspective of others. “To Kill a Mockingbird” is the story of the power of empathy.
Empathy can play a vital role in medicine, too, but when we don’t visualize what it is like to walk in our patients’ shoes, then we have a tendency to let them down. But being an empathic healer can mean diving far below the surface, and not settling for quick fixes and short-term gains. Truly being empathic can take time, but it also requires emotional energy, which can be taxing and sometimes uncomfortable.
Our country is now waging a very public debate on how to better regulate and prescribe opioid painkillers. When it comes to treating pain the government and the media is now entering the private sanctity of the doctor-patient visit in the exam room like never before. Concerns over the abuse of prescription painkillers has reached such a level that the CDC felt compelled to release stringent guidelines to doctors to curb the tide of the many tragic overdose deaths. Dr. Thomas Frieden, director of the CDC, went as far as to say that doctors rarely should ever prescribe opioids to patients for more than three days and that the “all-too-often-fatal risks far outweigh the unproven and transient benefits.”
On the heels of the CDC guidelines, CNN aired its town hall discussion“Prescription Addiction: Made in the USA,” hosted by Anderson Cooper and Dr. Sanjay Gupta, with a focus on the tragedies of addiction as opposed to the complexities of chronic pain. The experience of pain was marginalized and viewed as a secondary problem to the more pressing concern of medication addiction and misuse, with one expert talking about pain in the context of a “bruised knee.” But looking at painkillers only from the perspective of addiction really misses the deeper underlying reasons of why they get prescribed in the first place. From what I have heard and read, CNN’s town hall really raised the ire of pain patients and advocacy groups in a big way.
Why the outrage? Based on the feedback that I received, chronic pain sufferers feel disrespected and misunderstood by media coverage like the CNN town hall. They don’t appreciate being portrayed as drug seeking, and they widely argue that the real issue for them is the pain, not the pills. Comparing the plight of a long-time suffering pain patient on national television to a “bruised knee” is a punch in the gut, to be sure. In response, one patient advocate, who was in the audience but never asked to speak, griped to me later that “pain patients’ lives matter,” and another posted on my Facebook page that “CNN got it wrong.” A few days later I was a guest on a talk radio show in Cincinnati, and the host kept saying “you doctors should all be thrown in jail” because he felt people are just too soft when it comes to pain, noting that as a kid his dad made him finish a little league game with a broken leg. Hhhmmm…I wonder who should be thrown in jail here?
This brings me back to empathy, or the lack thereof. When I meet with a patient with a debilitating chronic pain problem of some sort, something that I have done on a daily basis for the last 20 years, I hear a very complex story containing many different but interlocking elements. As I often tell my patients, there are many layers to the onion when it comes to understanding their pain experience. There are physical pieces to the story, like injuries to the nervous system and musculoskeletal system, rendering the body a very limited and deconstructed version of its former self, struggling to walk or move. And there are the often overlooked psychological and spiritual components of the equation, like depression, anxiety, PTSD, fear, and hopelessness which constitute a major part of the suffering. I routinely see families torn apart by chronic pain, careers destroyed, and people even evicted without enough money for room and board, sometimes forced to live out of a car. Once I lean in and dive deeper, I often hear tragic personal stories of abuse and trauma that often precede the injuries people come to see me for. I can’t possibly know what it is really like to walk in these kinds of shoes, but it is my job to try if I am going to be of any value to the patient sitting in the chair in front of me.
Changing the dialogue between doctors and patients has to go beyond just saying no to requests for pain pills to yes – let me help you heal the hurt. Doctors now have tough decisions to make, but to do this right, we must cast our gaze far deeper than the bruise on the surface. Clearly, when doctors settle for just being a symptom manager as opposed to a creator of better health and wellbeing this fuels the painkiller crisis and fails those who need our help the most. Medicine can and should raise the bar higher than that. But everyone who is impacting the lives of those in pain, whether they are doctors on the front lines, pundits in the media, or even policy makers in Washington, should all heed the advice of Atticus and step inside the skin of pain.


